Naturopathic Doctors Adopt Evidence-Based Medicine, Study Finds

Published
Naturopathic doctors (NDs) increasingly embrace evidence-based medicine as part of their practice, according to a study by Bastyr University researchers published in the International Journal of Naturopathic Medicine.
The study asked naturopathic leaders about their attitudes toward evidence-based medicine (EBM), the philosophy that medical practice should be guided by the best available research data, balanced with a doctor's judgment and a patient's values. Those interviewed described a "rapid cultural shift" among NDs toward "cautious embrace" of evidence-based medicine, the authors wrote.
"I was glad to see the results," says co-author Jane Guiltinan, ND, dean of Bastyr's School of Naturopathic Medicine. "I came to naturopathic medicine from a conventional medical background and believe that, for naturopathic medicine to evolve and become more effective, the field needs to bridge the worlds of science and naturopathic philosophy. The study suggests that's happening."
It's a significant finding for a discipline sometimes seen in tension with scientific conventions. Naturopathic medicine rests on the philosophy of vis medicatrix naturae — the healing power of nature. While naturopaths have conducted and used clinical research for years, they stress that there are things conventional science cannot measure, such as the body's natural ability to heal. The findings suggest the profession is growing more comfortable integrating science and nature, says lead author Joshua Goldenberg, ND ('13).
"For me, the big message is not that there are different camps among naturopaths, but that this culture is changing rapidly," says Dr. Goldenberg, a recent graduate of Bastyr University's Doctor of Naturopathic Medicine program. "That's very exciting."
"Research is Self-Reflection"
The research team, funded by the Bastyr Center for Student Research, interviewed 15 naturopathic physicians and research leaders by phone and in person. The team found that much depended on how respondents defined evidence-based medicine. The more comprehensive they understood it to be, the more they trusted it. (Dr. Guiltinan describes evidence-based medicine as "scientific evidence, clinical judgment, and patient values, all weighted equally.")
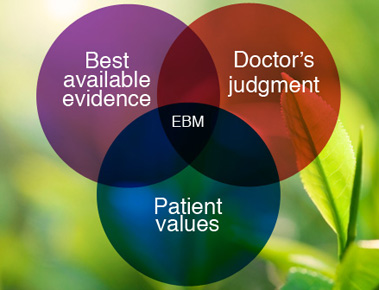 Once NDs understand that evidence-based medicine has room for a doctor's judgment and a patient's values, they become much more accepting, Dr. Goldenberg says.
Once NDs understand that evidence-based medicine has room for a doctor's judgment and a patient's values, they become much more accepting, Dr. Goldenberg says.
"When we really probed the people who had negative views about evidence-based medicine, they understood the definition was, 'Patient comes in with X and you always give them Y,'" he says. "No one really means that. That's the fear, but it's certainly not the intention of the founders of EBM."
The study found multiple reasons for the attitude shift, including the influence of leaders in the naturopathic world and a desire for credibility in conventional medicine. The growth of funding and institutions for naturopathic research was another key reason.
Some respondents gave poignant reasons for changing, such as working with AIDS patients.
“I'm going to float the idea that what substantially changed the attitude of 'We don’t have anything to prove, we can cure any disease,' was the AIDS epidemic," wrote one participant. "Any ND worth their salt was trying to help people who are HIV-positive and had developed AIDS. And I think everybody honest just realized we didn’t have any effective therapy.”
“Research is self-reflection,” wrote another. “We have to reflect on ourselves. Not everything we’re going to do is going to be perfect, and if you’re not willing to examine yourself, do you really deserve to be a doctor?”
The Art of Medicine
Dr. Goldenberg grew interested in naturopathic attitudes after his journey working in conventional science and discovering that healing requires more than science. He came to Bastyr after working as a molecular ecologist and passing up conventional medical schools (read the story of his epiphany). During his Bastyr studies, he discovered that the scientific dimension of medicine and the vis, or vitalistic dimension, are not exclusive — they aid each other. Balancing them became important as he began clinical training.
“When I first fell in love with the idea of EBM, I wasn't working in a clinical setting yet," he says. “To be in clinic, with real patients, you learn medicine is very artful and beautiful, but it's really a mess sometimes. You try to get everything better and do the best for your patient, but it's not this clean-cut cookbook where the patient comes in with X and you give them Y. That just doesn't happen in real life, and it wouldn't be good medicine."
He also learned that much conventional medicine relies on sparse evidence that is often later called into question. For example, medical doctors commonly use selective serotonin reuptake inhibitor drugs to treat depression. But a meta-analysis found they may be no more effective than a placebo for all but the most extremely ill.
To Dr. Goldenberg, that suggests medicine must always involve a doctor’s judgment, a patient’s values and an element of mystery.
Two Patients, Two Approaches
 Dr. Guiltinan also comes from a scientific background, studying medical technology as an undergraduate. As a faculty supervisor at Bastyr Center for Natural Health, the University's Seattle teaching clinic, she offered two stories that illustrate how the naturopathic field has changed — and how it remains distinct from conventional medicine.
Dr. Guiltinan also comes from a scientific background, studying medical technology as an undergraduate. As a faculty supervisor at Bastyr Center for Natural Health, the University's Seattle teaching clinic, she offered two stories that illustrate how the naturopathic field has changed — and how it remains distinct from conventional medicine.
1. A woman recently visited Bastyr Center after a stroke had sent her to the emergency room. ER doctors put her on pharmaceutical drugs for high blood pressure and cholesterol, and she needed help reducing the risk of another stroke.
At Bastyr Center, she met with a team of naturopathic medicine students who reviewed the evidence supporting her medications, along with their side effects and risks. They also considered herbal alternatives for blood pressure such as hawthorn berry, garlic and lime leaves. Because of the woman's high risk of another heart incident, they suggested she continue taking her medications, while also working to lose weight and lower cholesterol through dietary changes.
Their supervisor — Dr. Guiltinan — confirmed it was a responsible plan for a high-risk patient.
"In the past, students might have argued with me about that," she said. "But they reached this conclusion in their own independent research for this case."
2. That same day, another patient visited Bastyr Center looking for a second opinion on hormone-replacement therapy, which she had been using for three years for menopausal symptoms. Student clinicians reviewed the clinical evidence and suggested she taper off the hormone treatment, because it brings elevated risks after several years. After reviewing the plan with Dr. Guiltinan, they helped the patient make the transition with naturopathic methods of adrenal support, such as Siberian ginseng, ashwagandha and organic soy.
Those two examples provide a small picture of the path NDs can forge by integrating the best of their medicine with the most successful elements of conventional medicine, Dr. Guiltinan says. She wrote an editorial accompanying the attitudes study calling for NDs to embrace evidence-based medicine.
“It is the right thing to do for our patients,” she writes. “They deserve therapies that have been validated. The time to scrutinize what we believe and what we do with patients in a systematic way is here.”
----
Learn more about Bastyr's Doctor of Naturopathic Medicine program and research studies.